Bacterial meningitis also known as pyogenic meningitis is one of the potentially serious infection occuring in infants & older children. It becomes life threatening at times with high morbility & modality.
Commonest bacteria causing meningitis are Haemophilus influenzae, Streptococcus pneumoniae & Neisseria meningitides 1,2. Other bacterias causing bacterial meningitis are Group-b Streptococcus, staphylococcus pneumoniae, staphylococcus aurieaus & Klebesiella pneumoniae. Previously haemophilus influenzae Type-B accounted for up to 48% of all bacterial meningitis cases2; however, with the introduction of HIV vaccination, there is dramatic reduction in the incidence of Haemophilus meningitis.
The infection causes widespread meningeal exudates which extend to the cerebral vessels, venous sinuses, convexity meninges, sulci & sulvian fissures. This leads to congestion & hyperemia of the pia & arachnoid mater, distension of the subrachoid space & exudation with neurtrophils3. Involvement of the blood vessels causes spasm or thrombosis resulting in arterial & venous infarct4. Perivascular inflammation can extend to the brain parenchyma inducing cerebritis & abscess. There may be subdural effusion due to necrosis of the arachnoid granulation in some cases5. There may be hydrocephalus & ventriculitis.
In early cases of bacterial meningitis, clinical features are non-specific and include fever, malaise, headache and followed by neck stiffnsess, photophobia, phonophobia & vomitting etc6. Seizure may be the presenting symptom in few cases. In untreated cases, patient may develop complications leading to various sign-sign symptoms.
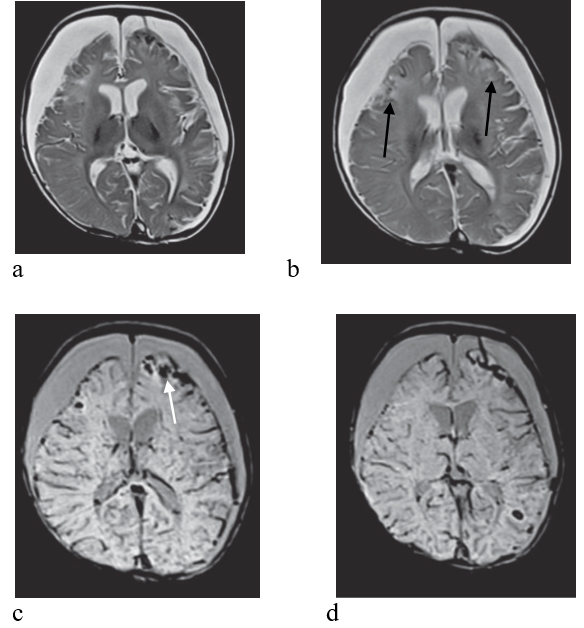
Imaging may be completely normal in uncomplicated cases of acute bacterial meningitis except mild edema in some cases. Small white matter infarcts may be visible, hence DW images are of utmost importance in detecting the early infarcts7. Hydrocephalus may occur in some cases, though it is relatively common in tubercular meningitis. Subdural hygroma & empyema are common complications of acute bacterial meningitis. It is very important to differentiate these two conditions as empyema requires aggressive treatment unlike hygroma which resolves spontaneously5. On precontrast T1 & T2 weighted images, both empyema & hygroma show similar signal intensity; however there is enhancement of the capsule in empyema. There is also diffusion restriction in empyema. Venous sinus thrombosis is another complication which occurs due to thrombophlebitis. On imaging there are filling defects in the cortical veins & venous sinuses. Superficial cortical vein is most commonly involved followed by superior sagittal sinus, deep cerebral veins, cavernous, straight & sigmoid sinuses in order of frequency. Involvement of the cortical vein cause venous infarct8, prominent vessels including bridging veins are also seen in some cases. There are haemorrhagic areas in the brain parenchyma & subdural spaces in severe cases.
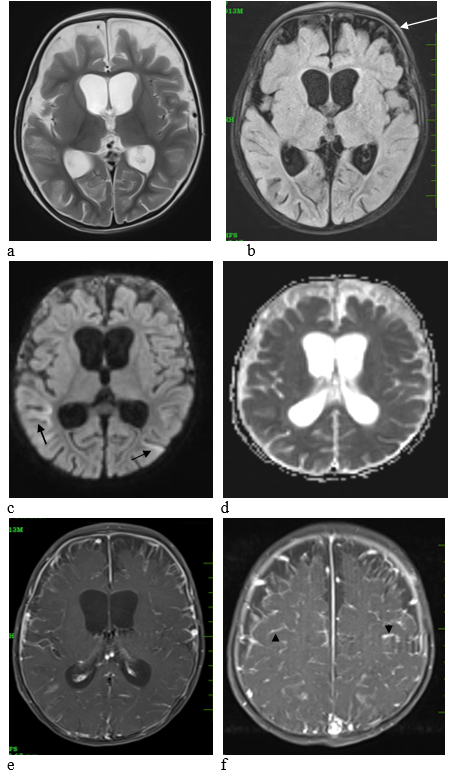
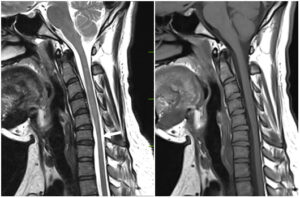
Figure:1 – 7 years old female patient of acute bacterial meningitis. There is widening of the frontal extraaxial CSF spaces with hydrocephalus, bridging veins (white arrow) seen traversing the widened extraaxial CSF spaces (a,b).There are diffusion restricting lesions (black arrow) in bilateral temporo-occipital regions suggesting acute infarcts (c,d). Post contrast study (e,f) shows numerous vessels, enhancing lepto-meninges (black arrow head).
References:
- Thigpen M, Whitney C, Messonnier N et al. Bacterial Meningitis in the United States, 1998-2007. N Engl J Med. 2011;364(21):2016-25. doi:10.1056/NEJMoa1005384 – Pubmed
- 4. McIntyre P, O’Brien K, Greenwood B, van de Beek D. Effect of Vaccines on Bacterial Meningitis Worldwide. Lancet. 2012;380(9854):1703-11. doi:10.1016/S0140-6736(12)61187-8 – Pubmed
- Parker JC Jr. Dyer MC. Neurologic infections due to bacteria fungi and parasitis. In: Doris RL. Roberston DM. eds Textbook of Neuropathology. Baltimore: Williams & Wilkins 1985: 632-703
- Hansman Whiteman ML, Bowen BC, Donovan Post MJ et. Al: Intracranial infection. In Scott W. Altas: Magnetic Resonance Imaging of the brain and spine Lippincott Williams and Wilkins 2002: 1099-1175
- Medhi N, Goswami P, Sarma P, Barkataky RK, Duarah R, Saikia R. Klebsiella meningitis. A case report. Neuroradiol J. 2008 Jun 3;21(3):323-6. doi: 10.1177/197140090802100305. Epub 2008 Jun 3. PMID: 24256900.
- Van de Beek D., de Gans J., Spanjaard L., Weisfelt M., Reitsma J.B., Vermeulen M. (2004) Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med 351:1849–1859 [PubMed]
- Jan W, Zimmerman RA, Bilaniuk LT et Al: Diffusion weighted imaging in acute bacterial meningitis in infancy. Neuroradiology 45: 634, 2003.
- Shahrzad,S Deliran,D.vandeBeek@amsterdamumc.nl, Matthijs,C Brouwer & Diederik van de Beek. Bacterial meningitis complicated by cerebral venous thrombosis, European Stroke Journel, Volume 5, Issue 4, December 2020, Pages 394-401